Malaria is a devastating infectious mosquito-borne disease caused by single-celled parasites called Plasmodium that can live inside red blood cells. In 2013, 500,000 people died after being infected with malaria. [1] As the malaria parasite mutates, it is becoming resistant to even the most powerful antimalarial drugs, such as artemisinin. [2] Malaria is also a health concern for deployed soldiers, as troops have been infected in Middle Eastern countries and during the effort to help prevent the spread of Ebola in West Africa.
In 2011, 124 U.S. military troops were diagnosed with malaria. Of those, 91 were linked to Afghanistan, 24 to Africa, four to South Korea and five unknown. [3] Since 2005, more than 800 troops have been diagnosed with malaria, and more than half of those cases originated in Afghanistan. [4]
Researchers at Washington University School of Medicine in St. Louis believe they may have found a new way to treat malaria by using luminol, the compound commonly used by detectives at crime scenes in order to find trace amounts of blood.
“The light that luminol emits is enhanced by the antimalarial drug artemisinin,” said Daniel Goldberg, MD, Ph.D., professor of medicine and microbiology at Washington University. “We think these agents could be combined to form an innovative treatment for malaria.” [5]
Luminol works by glowing blue when it encounters the hemoglobin in red blood cells. The new approach targets proteins made by human red blood cells, which the parasite is unable to mutate. Malaria parasites require heme, a component of hemoglobin, to survive. The scientists are giving a precursor to heme to malaria-infected red blood cells. The red blood cells change the precursor into a molecule, which when exposed to light emits dangerous, chemically reactive compounds called free radicals, killing the parasites. [5]
The research team plans to test this approach in animal studies.
“All of these agents—the theme precursor, the luminal and artemisinin— have been used in humans, so hopefully using the three of them together won’t present any safety problems,” said Goldberg. [5]
New methods for treating malaria are important worldwide because in many poor and developing tropical and subtropical countries it is a leading cause of death and disease. [6] Furthering malaria treatment and prevention options is important to the U.S. military as well because soldiers are routinely deployed to these locations. During the military deployment to aid with the Ebola crisis in West Africa in 2014, five soldiers were diagnosed with malaria upon their return to the United States. [4]
The soldiers recovered, but Army Surgeon General Lt. Gen. Patricia Horoho told the House Appropriations Committee defense panel that malaria “may be the number one threat” for deployed service members. [4] The U.S. Army Medical Research and Materiel Command recognizes a need for new anti-malarials due to increased drug resistance, as well as more ideal vaccines and more effective mosquito avoidance. [7]
“When you look at the missions in which we are deploying more and more to, the threat of malaria is one of the biggest, if not the number one threat,” Horoho said.[4]

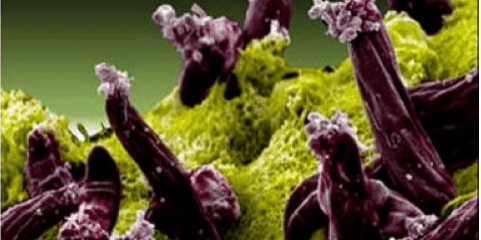
Photo showing parasite-infected red blood cell treated with the new luminol, antimalarial combination. The cell glows red when light is shined on it because of the accumulation of protoporphyrin IX in the cell. (Image courtesy of Dan Goldberg, Washington University in St Louis)
References:
[1] Centers for Disease Control. Malaria.
[2] National Institutes of Health. (2014, February) Study shows parasite mutation behind drug-resistant malaria in Cambodia. Global Health Matters.
[3] Gould, Joe. (2012, February 22). Malaria cases up among soldiers in Afghanistan. Army Times.
[4] Kime, Patricia. (2015, April 23). Troops get malaria during Ebola deployment. Military Times.
[5] Purdy, Michael C. (2015, August 6) Crime-scene compound may be newest tool in fight against malaria.
[6] Centers for Disease Control. Impact of Malaria.
[7] The Walter Reed Army Institute of Research. Malaria and Leishmaniasis Drug Development. Soldier Health World Health.